Scientists Used CRISPR to Edit a Gene That Causes Miscarriages
Credit to Author: Mallory Locklear| Date: Mon, 02 Oct 2017 15:14:59 +0000
Between 15 to 20 percent of pregnancies in the US will end in a miscarriage and when the cause isn’t known, it’s thought that genetics are often the culprit. Reproduction is a very complex process with an astounding number of factors at play. “The tricky thing about early development is there are so many things that can go wrong,” David Keefe, a fertility specialist at New York University, told me. “All happy embryos are the same and all unhappy embryos are unhappy in their own way.”
Because of that, figuring out the genetic causes underlying miscarriages has been incredibly hard to do. Some experiments compare the genomes of fertile and infertile adults and try to spot genetic differences between the two. But as Cornell University genetics professor John Schimenti told me, “There are so many different causes that the statistics aren’t great enough to identify common alleles in the population.”
CRISPR, a fairly new gene editing tool, is changing that. While it’s still a long way from preventing miscarriages, researchers have been using the technology to generate new methods of peeking into the genetics behind infertility in hopes of more successfully treating its causes.
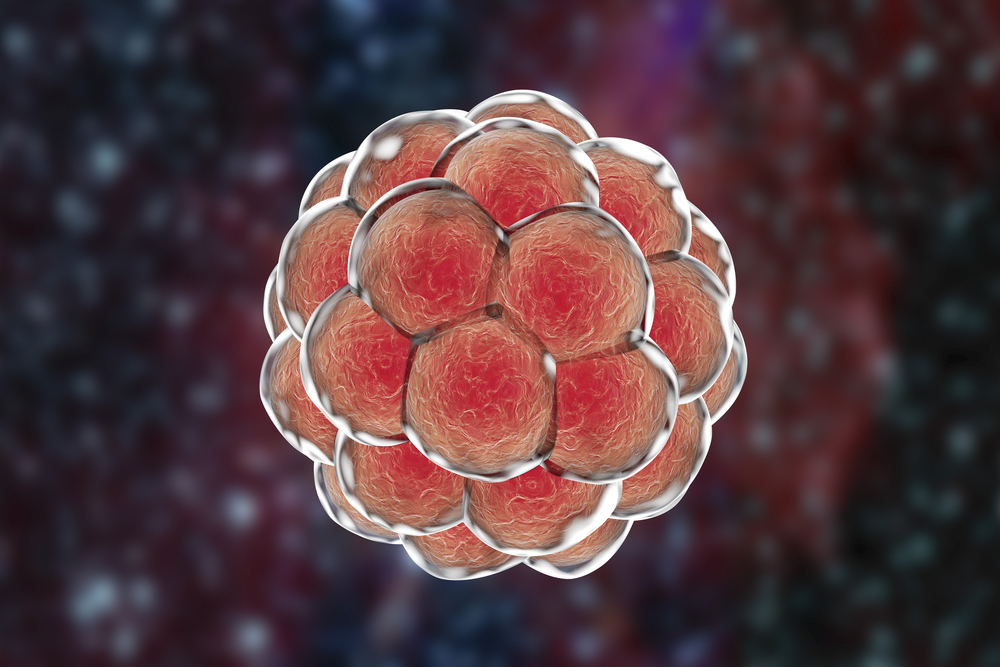
A recent Nature study from researchers at the The Francis Crick Institute in the UK demonstrated that CRISPR could be used to understand how certain genes impact the early development of human embryos. The team used CRISPR to successfully stop a gene from producing a key protein called OCT4, causing embryos to collapse. It’s the first time such a study has been done in human embryos.
“The impact that we think this type of work could have on fertility is more on how it could improve the treatment for infertility,” said Alessandro Bertero, a researcher on the project and a postdoc at the University of Washington, who notes that treatments like in vitro fertilization (IVF) aren’t terribly successful. Success rates can be as low as 15 percent depending on a woman’s age.
For this study, researchers used excess embryos donated from couples who completed IVF treatment, which is where most research embryos come from. But there are only so many of those, which is why animal studies are still important. In fact, mice still played a major role in this study too: Bertero’s role was to help optimize techniques in mice before the team ever touched a human embryo.
Bertero notes that in many cases, mice are still the best model for studying infertility. And Schimenti has also developed a method that brings mouse studies nearly as close to human studies as possible. He and his team took mutations found in human genes that were thought to be associated with infertility, then used CRISPR to introduce those same mutations into nearly identical genes in mice. “So, introduce the human mutation in the mouse and ask if it does something bad,” said Schimenti.
Those findings will help inform fertility treatments and hopefully bring their success rates up.
However, there’s still a big role here for human embryo studies. For example, while OCT4 is important for early development in both mice and humans, Bertero’s colleagues showed that it’s required much earlier in humans than mice.
With CRISPR we stand to learn a lot about infertility through both human embryos and mice. And those findings will help inform fertility treatments and hopefully bring their success rates up.
There are limitations, of course. First, there are a lot of genes to study and scientists are just getting started. Plus, there are a limited number of human embryos available for study and each one needs to be treated and used ethically. Along with spending months optimizing their methods, Bertero and his colleagues also discussed the project for years before doing it, adhered to the field’s standards of embryo use, and informed donors exactly what was to be done before they agreed to donate.
Keefe says researchers should proceed, but should do so with caution and thoughtfulness. “One experimental blunder can affect generations,” he said.
Other limitations in the US include funding sources. The National Institutes of Health, the biggest funder of biological research, will not fund studies that use human embryos due to ethics and unknown safety issues. But that hasn’t stopped some, like the US group that recently used CRISPR to remove a cardiac disease-causing mutation from a human embryo (though there’s some debate about their success). And a handful of teams around the world are also working on gene editing in human embryos.
Although, like any technology, it has limitations, CRISPR is set to vastly advance our understanding of early human development and fertility. And it’s not unlikely that we will eventually have one more option when choosing to have a child. In regards to the role CRISPR will play in the future of fertility, Keefe said, “It will be essential, really essential.”
Get six of our favorite Motherboard stories every day by signing up for our newsletter .